
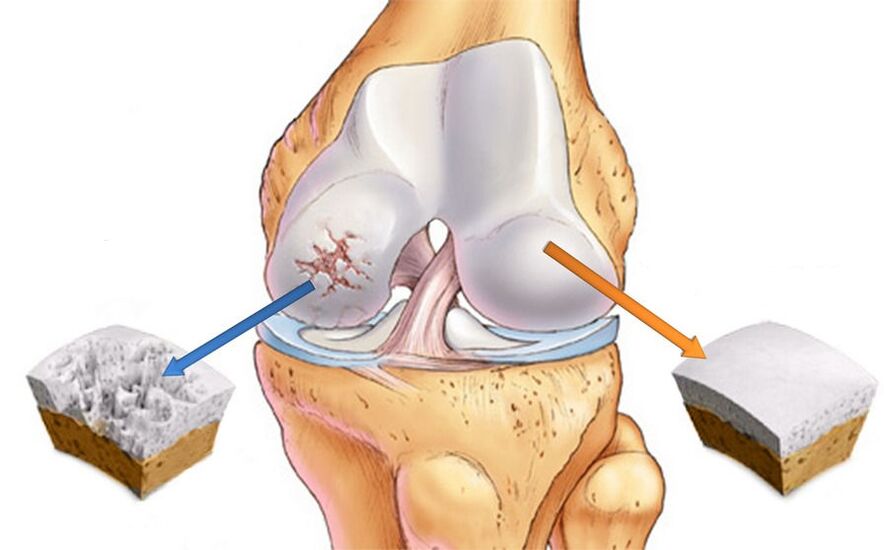
Osteoarthritis is a joint pathology that is accompanied by damage to the cartilage tissue. Synonyms for osteoarthritis are gonarthrosis, deforming osteoarthrosis, osteoarthritis; All these terms mean the development of degenerative processes in the cartilage that covers the epiphyses of the articulated bones.
Although the injury affects only the cartilaginous structures, all joint elements are affected: the capsule, the synovial membrane, the subchondral bones, as well as the ligaments and muscles that surround the joint. Osteoarthritis can affect one joint or several.
The most common localized forms of the disease have their own names: arthrosis of the hip joint is called coxarthrosis, arthrosis of the knee joint is called gonarthrosis.
Classification and reasons.
Knee osteoarthritis can be primary or secondary. The first group includes pathologies whose cause has not been established, that is, they are idiopathic. Secondary osteoarthritis occurs after injury, due to congenital anomalies and in the context of systemic diseases.
The following are the causes of osteoarthritis of the knee joint:
- autoimmune pathologies – rheumatoid arthritis, lupus erythematosus, scleroderma, etc. ;
- inflammation of the joints caused by a specific infection (syphilis, gonorrhea, encephalitis);
- hereditary diseases of the musculoskeletal system and joints, type 2 collagen mutations.
There are also a number of factors that negatively affect the joints and can cause pathological changes in them:
- old age, excess weight, osteoporosis;
- hormonal changes, including a decrease in estrogen synthesis during the postmenopausal period in women;
- Metabolic disease;
- deficiency of microelements and vitamins in the diet;
- congenital and acquired deformities of skeletal bones;
- hypothermia and poisoning with toxic compounds;
- constant injury to the joint during sports training or hard work;
- operations on the knee joint, for example, to remove the meniscus.
Symptoms and stages.
Deforming osteoarthritis of the knee joint is characterized by intracellular changes at the morphological, molecular, biochemical and biomechanical levels. The consequence of the pathological process is the softening, the formation of fibers and the reduction in the thickness of the articular cartilage. In addition, the surfaces of the bones that form the joints become denser and bony spines (osteophytes) appear on them.
DOA of the knee joints develops in 3 stages, and in the early stages it may manifest only minor pain and discomfort after prolonged physical activity. Sometimes one of the characteristic symptoms of osteoarthritis appears: morning stiffness. At this time, changes occur in the synovial membrane and the composition of the intra-articular fluid.
As a result, the cartilage tissue does not receive enough nutrients and its ability to resist pressure begins to decrease. Therefore, with intense exercise and long walks, pain occurs.
In the second stage of osteoarthritis, the destruction of cartilage tissue progresses and part of the increased load is assumed by the articular surfaces of the bones. Since there is not enough supporting surface, the edges of the bones increase due to osteophytes. The pain no longer goes away at rest like before and bothers me even at night.
The time of morning stiffness also increases and it takes a long time to "train" the leg to be able to walk normally. Also, when the limb is bent, crackling and clicking sounds are heard, accompanied by sharp pain. It is not always possible to bend the leg completely, it seems to be stuck, and subsequent attempts end in a sharp crunch and pain.

Due to the appearance of pain during any movement, a person tends to move less, which negatively affects the muscles surrounding the joint. A change in the size of the bone epiphyses causes a displacement of the axis of the limb and the development of deformity. The joint capsule becomes stiffer as the volume of fluid it contains decreases. When osteophytes compress the surrounding soft tissues, synovitis and chronic inflammation occur.
Moving into the third stage, the signs of osteoarthritis of the knee joint become very severe: the pain does not go away even at night, motor skills practically stop, the leg looks twisted and does not bend. The third degree of osteoarthritis is characterized by an X- or O-shaped deformity, which makes movement extremely difficult. An advanced form of gonarthrosis deformans can only be treated surgically.
Diagnosis
Diagnosing osteoarthritis of the knee joint is not particularly difficult; The doctor can assume gonarthrosis based on the existing symptoms and characteristic visual signs. To confirm the diagnosis, x-rays are performed. The images will show narrowing of the joint space, bone growths, and subchondral osteosclerosis of the bones.
X-rays are used to determine the cause of the disease. Bone deformations are especially visible in post-traumatic osteoarthritis. If cartilage degeneration is caused by arthritis, defects are detected along the edges of the bones, as well as periarticular osteoporosis and atrophy of bone structures. With various congenital anomalies, a distortion of the axis of one of the bones is observed, which led to improper distribution of the load and the appearance of secondary osteoporosis.
Treatment
Treatment of gonarthrosis of the knee joint has 3 main goals: restoring cartilage tissue, improving joint mobility and slowing down the progression of the disease. Great importance is attached to the elimination or attenuation of symptoms, reducing the intensity of pain and inflammation. Medications, physical therapy, and exercise therapy are used to solve these problems. To obtain the maximum effect of therapy, dosed physical activity and compliance with the orthopedic regimen are necessary.
The pharmacological treatment of knee osteoarthritis includes taking analgesics and anti-inflammatories, as well as chondroprotectors that promote the regeneration of cartilage tissue. Medications can be prescribed in the form of injections, tablets, ointments and gels.
If first degree knee osteoarthritis is diagnosed, physiotherapeutic methods, physiotherapy and massage are used in the treatment. The early stages of the disease are much easier to treat and a full recovery can be expected. An important condition is to lose weight to reduce the load on the sore joint.
Treatment of osteoarthritis of the knee joint of the second stage necessarily includes exercise therapy, the use of orthopedic devices and following a diet. To relieve pain, non-steroidal anti-inflammatories, chondroprotectors and intra-articular injections of hyaluronic acid are prescribed.
Acute osteoarthritis is characterized by severe pain, for which conventional NSAIDs are not sufficient. In this case, strong analgesics and injection of glucocorticosteroids into the joint cavity are used.
If conservative methods are not effective, an operation is performed, which can be corrective or radical (replacing a joint with a prosthesis).
Deforming osteoarthritis of the knee joint of the third stage is characterized by the complete absence of the interarticular space, replaced by a bone structure. This condition requires surgical intervention, since other methods in this case are powerless.
NSAIDs and corticosteroids
To save patients from physical and mental suffering, therapy for acute osteoarthritis begins with pain relief. Medications that are part of the NSAID group and can be used in tablets or topically have been shown to be effective.
The analgesic effect does not always occur immediately, but after two or three days it reaches its peak and the pain disappears. The NSAID treatment course is limited to two weeks, as prolonged use increases the risk of side effects. Particular caution should be taken with people who have problems with the gastrointestinal tract, as well as those suffering from high blood pressure.
If there is no result, hormonal drugs are prescribed to relieve inflammation. In the case of left-sided gonarthrosis, drugs are injected into the left knee, and into the right knee - into the right.
Hormonal injections can be given once every 10 days, not more frequently. The indication for such treatment is a large accumulation of fluid in the joint due to inflammation. As the symptoms disappear, they switch to medications in tablet form.
Chondroprotectors and hyaluronic acid
Chondroprotective agents act in three directions: they restore damaged cartilage tissue, reduce pain and eliminate inflammatory reactions. Taking chondroprotectors helps to normalize the composition and properties of synovial fluid, nourish cartilage and protect pain receptors from irritation.
As a result, the destruction of cartilage structures and, consequently, the progression of the disease slows down. After treatment with medications, the cushioning and lubricating function of the joint is restored.
In the early stages of the disease, chondroprotectors in the form of ointment or gel can be used. However, intra-articular injections are the most effective. Modern methods of treating osteoarthritis include the use of combined agents, which contain not only chondroprotective substances, but also anti-inflammatory components and vitamins.
Hyaluronic acid is the main component of synovial fluid, responsible for its viscosity and consistency. It is, in fact, a biological lubricant that provides elasticity, elasticity and resistance to cartilage.
With the development of joint pathologies, the volume of hyaluronic acid can decrease by 2-4 times, which necessarily leads to excessive friction of the bones. With intra-articular injection of hyaluron, knee function is normalized and the person can move normally.

Surgery
Surgery is a radical method by which the functionality of the joint is fully or partially restored. The degree of intervention may be different and depends on the stage of osteoarthritis. The most gentle operation is arthroscopy: the rehabilitation period after its implementation is the least painful for the patient.
Important:Arthroscopy can be performed not only for treatment, but also to diagnose joint pathology. This procedure allows you to identify damage that is inaccessible to other studies.
The goal of arthroscopy is to prolong the life of the joint by removing dead and damaged tissue from the joint cavity. As a result, pain disappears, stress resistance increases, and motor activity returns.
In case of significant deformities, osteotomy is indicated, creating an artificial bone fracture in a specific area. Knee osteotomy literally means "cutting the bones": during the operation, the surgeon removes a wedge-shaped segment of the femur or tibia and then combines the bones in the most physiological position. If necessary, the resulting space is filled with bone graft. During the healing period, the structure is fixed with special clamps.
Endoprosthesis replacement is an alternative method to the outdated arthrodesis procedure, the essence of which is the partial or total replacement of a diseased joint with a prosthesis. As a result, knee function is completely restored in more than 90% of cases, significantly improving patients' quality of life.
Physiotherapy
Physiotherapeutic procedures play an important role in the treatment of osteoarthritis due to their beneficial effect on damaged joints. A course of physiotherapy accelerates regeneration processes, eliminates pain and muscle spasms. Additionally, certain procedures allow administration of drugs through the skin, thus reducing the dose of oral drugs.
For damaged joints, the following techniques are recommended:
- magnetic therapy;
- medium wave ultraviolet (WUV);
- infrared laser;
- ultrahigh frequency;
- ultrasound;
- diadem and sinusoidal modulated currents (amplipulse therapy);
- Darsonval.
Effective treatments for osteoarthritis are also therapeutic baths: radon, hydrogen sulfide, bischofite, mineral and sage. They have an anti-inflammatory, analgesic and joint repairing effect.
Finally
If knee osteoarthritis is suspected, an orthopedic or traumatologist should be consulted to diagnose and treat these pathologies. In order not to aggravate the disease, it is necessary to avoid excessive physical activity on the legs and get rid of excess weight.
There is no special diet for osteoarthritis, but it is recommended to avoid concentrated meat and fish broths, fatty meats and smoked meats, and also reduce the consumption of table salt. The diet should be dominated by foods rich in vitamins and minerals and vegetable oils. In addition, once a week it is advisable to organize a fasting day: kefir, cottage cheese or fruits and vegetables.
To strengthen the muscular corset of the lower extremities and increase blood flow, it is necessary to regularly perform therapeutic exercises, which are individually selected by a physiotherapy instructor.
Thus, taking medications, physical procedures, a balanced diet and physical exercise are what will definitely help a patient with osteoarthritis. And to avoid traumatic surgery, it is advisable to seek medical help as soon as possible. Be healthy!

























